Differences Between TMS and tDCS in Non-Invasive Brain Stimulation
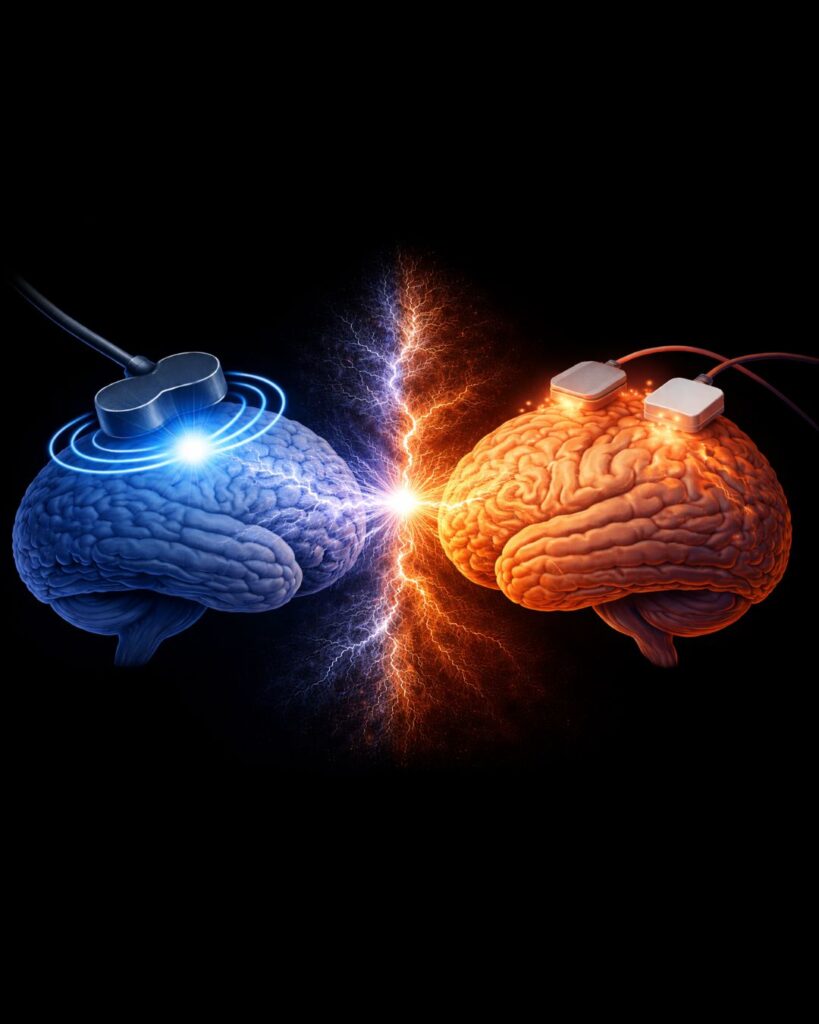
Non-invasive brain stimulation (NIBS) has become a central topic in modern neuroscience. Among available techniques, Transcranial Magnetic Stimulation (TMS) and Transcranial Direct Current Stimulation (tDCS) are the most widely used in both research and clinical contexts.
Despite their conceptual similarity, these two methods differ substantially in terms of mechanisms of action, level of scientific evidence, and clinical applicability.
Introduction
In recent years, non-invasive approaches for studying and modulating brain function have expanded considerably. Both TMS and tDCS can be applied without surgery or direct penetration of brain tissue; however, their neurophysiological effects and intended purposes are fundamentally different.
Understanding these distinctions is essential for researchers and clinicians working in neuroscience and neuropsychiatry.
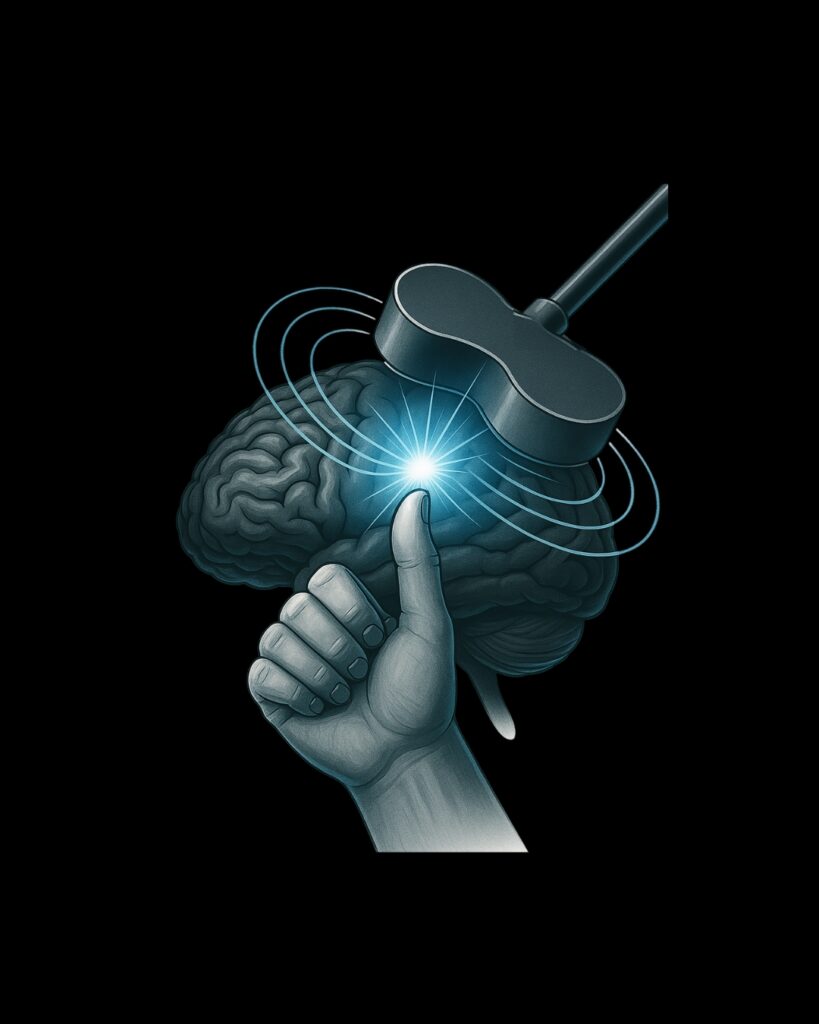
What Is TMS? (Transcranial Magnetic Stimulation)
Transcranial Magnetic Stimulation is based on the principle of electromagnetic induction. Brief magnetic pulses generate electric currents in the cerebral cortex, leading to direct neuronal depolarization and activation. Initially introduced as a research tool, TMS gradually evolved into a clinically applicable technique.
For a detailed discussion of its development and clinical integration, see: “The History of TMS: From the First Muscle Twitch to Clinical Applications.”
What Is tDCS? (Transcranial Direct Current Stimulation)
Transcranial Direct Current Stimulation delivers a weak, continuous electrical current through surface electrodes placed on the scalp.
Unlike TMS, tDCS does not usually trigger direct neuronal firing; instead, it modulates neuronal membrane potential, thereby increasing or decreasing cortical excitability over time.
Differences in Mechanisms of Action
The primary distinction between TMS and tDCS lies in how they interact with neural tissue:
-
TMS: Magnetic fields induce rapid electrical currents, resulting in direct neuronal depolarization.
-
tDCS: Weak electrical currents shift neuronal excitability without eliciting action potentials.
These mechanistic differences underpin their divergent research and clinical roles.
Spatial Specificity and Regional Control
TMS
Evidence from neuroimaging and modeling studies indicates that TMS offers higher spatial specificity, allowing targeted stimulation of discrete cortical regions.
tDCS
In tDCS, electrical fields are distributed more diffusely across the brain, resulting in broader, network-level effects rather than focal stimulation.
Clinical and Research Applications
Based on current scientific evidence:
-
TMS is supported by standardized clinical protocols and controlled clinical trials.
-
tDCS is predominantly used in cognitive neuroscience research and as an adjunctive or exploratory intervention.
TMS and tDCS in the Treatment of Disorders
In clinical neuroscience, a technique is considered a treatment only when it demonstrates reproducible efficacy and standardized therapeutic frameworks.
Within this context:
-
TMS is recognized as an evidence-based clinical treatment for specific indications.
- tDCS remains primarily a research or modulatory tool and is not considered a standalone standard treatment.
Conclusion
Although both TMS and tDCS are non-invasive brain stimulation methods, they differ fundamentally in mechanism of action, spatial specificity, strength of evidence, and therapeutic role.
At present, TMS has received FDA approval for specific clinical indications and is used as an evidence-based treatment in clinical practice.
In contrast, tDCS does not have FDA approval as a standard therapeutic intervention and is mainly explored within research and adjunctive frameworks.
Understanding these distinctions supports informed decision-making in both neuroscience research and clinical applications.
| Feature | TMS | tDCS |
|---|---|---|
| Mechanism of Action | Electromagnetic induction leading to direct neuronal depolarization | Modulation of neuronal excitability without direct firing |
| Spatial Precision | Focal and targeted | Diffuse and network-level |
| Strength of Neuromodulation | Stronger and more controlled | Mild and gradual |
| Depth of Effect | Significant penetration into cortex | Primarily limited to cortical surface |
| Evidence Base | Supported by standardized clinical protocols and RCTs | Mostly exploratory or adjunctive research use |
| FDA Approval | Yes (for defined indications) | No standard FDA approval |
| Patient Sensation | Mild tapping/pressure on scalp | Mild tingling or itching sensation |
| Durability of Effect | Longer-lasting and more durable | Short-term and dependent on repeated sessions |